Disc herniation is a health condition that can affect people of all ages, causing intense pain in the lower back, buttocks, legs, or arms.
What is a disc herniation?
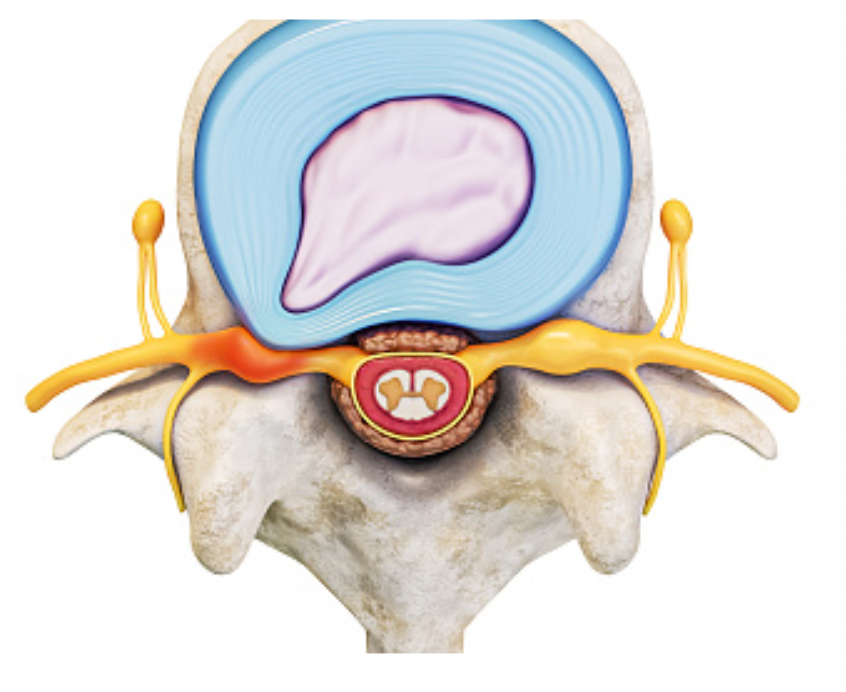
It is a medical condition that occurs when a part of the intervertebral disc, which usually acts as a cushion between the spinal column’s vertebrae, protrudes beyond its normal position and presses on the adjacent nerve roots or spinal cord. This can lead to symptoms such as back pain, numbness, tingling, or weakness in the affected limbs. A herniated disk can occur in any part of the spinal column. Still, they are most common in the lumbar and cervical regions. In more severe cases, treatment may include conservative therapies such as physical therapy, pain medication, or surgery.
Understanding the Spinal Column
It is essential to understand that the spinal column is formed by joints composed of vertebrae between intervertebral discs. These discs comprise a fibrous ring and a gel-like nucleus called the nucleus pulposus. The discs are responsible for supporting the weight of the body and all the movements you make, such as bending and rotating the spine. Their function is to cushion and absorb the spine’s impacts daily. The spinal column is divided into:
- Cervical
- Thoracic
- Lumbar
- Sacral
- Coccygeal
The cervical and lumbar regions are the most commonly affected by a herniated disc.
Types of Herniated Disc
There are several types, classified based on their location in the spinal column and the direction of the disc protrusion. Some common types include:
Cervical – occurs in the neck region (cervical spine).
Thoracic – occurs in the upper back region (thoracic spine) and neck disc herniation.
Lumbar – occurs in the lower back region (lumbar spine).
Extruded disc herniation – when the disc material exits its common space but is still connected to the disc.
Sequestered disc herniation – when the disc material completely exits the disc and becomes free within the spinal canal.
Protruded disc herniation – when the disc material protrudes beyond its normal position but is still connected to the disc.
Paracentral disc herniation – occurs when the disc protrusion is close to the center of the spinal cord.
Causes of Disc Herniation
Disc herniation can arise due to natural wear and tear of the intervertebral discs that occurs with aging, an injury, or spinal column trauma. Some factors that can contribute to the development of disc herniation include:
Mechanical overload: Engaging in repetitive movements or heavy lifting activities can gradually wear down the intervertebral discs and cause a herniation.
Aging: The intervertebral discs, with age, lose water and become less flexible, increasing the likelihood of disc herniation.
Genetics: Some studies suggest that specific individuals may be more predisposed to developing disc herniation due to genetics.
Poor posture: Maintaining a seated or standing position with poor posture can exert excessive pressure on the spinal column and increase the risk of disc herniation.
Smoking: Smoking can reduce blood circulation to the intervertebral discs and increase the risk of disc herniation.
Symptoms of Disc Herniation
The symptoms of disc herniation can vary depending on the location and severity of the herniation. Common symptoms may include:
Back or neck pain can be localized or radiating depending on the affected spinal area.
Numbness and tingling: The compression of nerves can lead to numbness and tingling in the arms, legs, or other body parts.
Muscle weakness: Weakness in the muscles supplied by the affected nerves may occur, leading to difficulty performing specific movements or activities.
Radiating pain: If the herniated disc compresses a nerve root, it can cause pain that radiates along the path of the nerve. For example, a herniation in the lumbar spine may cause sciatica, characterized by pain radiating down the leg.
Loss of bladder or bowel control: In severe cases where the herniated disc compresses the spinal cord, it can lead to a loss of bladder or bowel control. This is a severe symptom that requires immediate medical attention.
Diagnosis and Treatment
If disc herniation is suspected, a healthcare professional will typically conduct a thorough physical examination and review the patient’s medical history. Diagnostic imaging tests such as X-rays, MRI (Magnetic Resonance Imaging), or CT (Computed Tomography) scans may be ordered to visualize the spinal structures and confirm the diagnosis.
The treatment approach for disc herniation depends on the severity of symptoms and the individual’s specific condition. Initially, non-surgical treatments are typically recommended, including:
Rest and activity modification: Avoid activities that exacerbate symptoms and allow the body time to heal.
Pain medication: Over-the-counter or prescription pain medications may be used to manage pain and inflammation.
Physical therapy: Specific exercises and stretches can help strengthen the surrounding muscles, improve flexibility, and alleviate symptoms.
Epidural steroid injections: In some cases, corticosteroid injections may be administered to reduce inflammation and relieve temporary pain.
Surgical intervention may be considered if conservative treatments do not provide sufficient relief or if the herniation is severe and causing significant neurological deficits. Surgical options may include discectomy (removing the herniated disc material) or spinal fusion (joining vertebrae to stabilize the spine).
It’s important to note that a qualified healthcare professional should determine the specific treatment plan based on an individual’s unique circumstances.
Remember, this information is intended for educational purposes only, and it’s always best to consult with a healthcare professional for accurate diagnosis and personalized advice.
References:
Read more: Disc Herniation: Causes for Intense Back Pain